How Can Pelvic Floor Exercises Prevent Pelvic Organ Prolapses?
The pelvic floor is a group of thick, strong muscles and ligaments that sit at the bottom of the pelvic area. Their job is to hold all of the pelvic organs in place, by acting as a muscular hammock. However, like all muscles in the body, if you don’t exercise them, then you lose them. If the pelvic floor muscles become weak and loosen, then they can no longer do their job as effectively. A weak pelvic floor is the leading cause of pelvic organ prolapses.
Pelvic floor, or Kegel exercises are designed to keep the pelvic floor muscles strong. They’re the best defence both against a pelvic organ prolapse, or if you already have one, preventing it from getting any worse and strengthening the muscles to bring the organ back into position. Even if a pelvic organ prolapse is so severe that it requires surgery, daily Kegel exercises need to be continued to help prevent it from recurring and to aid your recovery.
There are many things which can cause your pelvic floor to weaken. Take a look at our causes and symptoms page to learn more.
Other Benefits of Having a Strong Pelvic Floor
Not only does having a strong pelvic floor reduce your risk of developing a pelvic organ prolapse. It can also:
- improve sensation and orgasms during sex
- improve the control you have over when and where you empty your bladder and bowel
- improve childbirth
- add strength to your core which can lead to a flatter tummy
- relieve back pain
- improve your posture
How Can You Find Your Pelvic Floor?
It can be tricky locating your pelvic floor muscles because your pelvic floor is hidden from view. Here are our top tips on finding your pelvic floor muscles, so that you can exercise them properly:
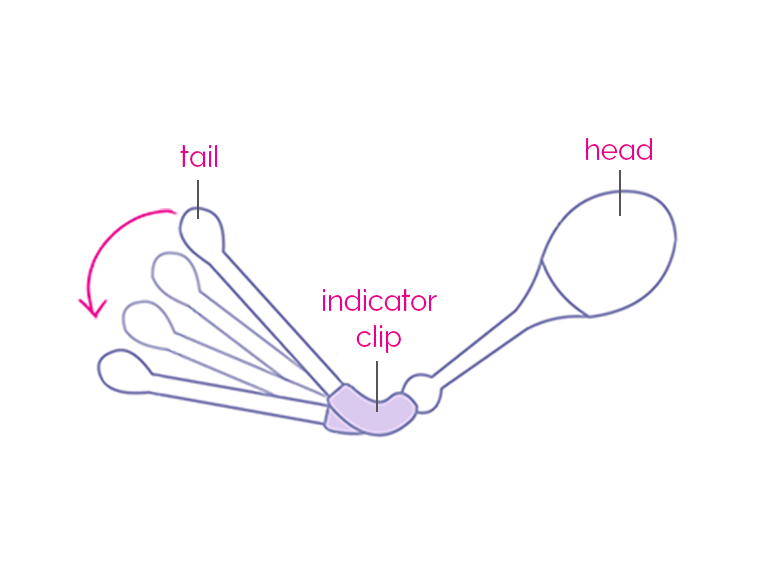
- Use a Kegel8 Vaginal Cone to know when you are contracting the correct muscles. The unique indicator will dip down when you have it just right; shown in the image here.
- When you’re passing urine, try to stop mid-stream. If you can stop urinating, then congratulations, you’ve found your pelvic floor muscles! If you already have a bladder prolapse then you may not be able to stop your urine stream mid-flow, but if you make the action to at least try and stop it, then you’re doing just as well!
- A prolapse can also affect the rectum, so it’s crucial to also train the pelvic floor muscles at the back of the pelvis as well as those at the front. Try to imagine that you’re about to pass wind, and that you desperately want to keep it in. The muscles that you’re using right now to squeeze that wind back up, are your pelvic floor muscles. Exercising these will help to strengthen those around the rectum, and those around the bladder and vagina.
- Using a mirror to visualise where they are can also help. Hold a mirror under your pelvis and look at the area between your vaginal opening and your anus. This is called the perineum, a muscular wall that is connected to the pelvic floor muscles. Now squeeze the muscles that you’ve just located by holding in urine and wind. You should see the perineum lift up as you squeeze.
- You can also feel them at work too. Sit or lay down and place a finger inside your vagina. Now squeeze those pelvic floor muscles. You should feel a tightening around your finger, along with a lifting sensation. If you have a prolapse, then you might not feel this, but as you begin to perform your Kegel exercises daily, you will begin to notice a tightening and a lifting as the months go by. This is a great way to measure the success of all your hard work! If you have a prolapse that protrudes from the vagina, get used to gently pushing it back up into your vagina before performing your Kegel exercises.
How to do Kegel Exercises
The muscles of the pelvic floor aren’t exercised just by walking or by any other kind of common exercise. In fact, they can be weakened by lots of high impact training such as long distance running and plyometrics (jump training). although maintaining a healthy weight and a BMI of under 30, will help.
Performing Kegel exercises couldn’t be simpler, you can perform them during your normal day-to-day life, and no one will know you’re doing them! Now that you know how to find your pelvic floor muscles, here’s how to train them:
- Lay down, pull in and squeeze your pelvic floor muscles by pretending you’re holding in urine and gas at the same time.
- Hold that squeeze for three seconds remembering to continue breathing.
- Relax for three seconds (note that relaxing is just as important as the squeeze so you don't cause your muscles to get over-tight).
- Repeat ten times, three times a day (or more frequently if you’ve been advised to).
- Gradually increase the time that you hold the squeeze for until you reach a full ten second squeeze each time.
- When you’re an expert, carry out these exercises whilst sitting or standing as well as laying down. Being at your desk or waiting at the train station is no barrier to your success!
Here are some additional steps you can take to help even more:

- If you’re unsure that you’re doing them right, you can use biofeedback tools such as vaginal cones or electronic biofeedback trainers to see if you are using the muscles correctly. Shown in the image here.
- Breathe as you squeeze, don’t get into the habit of holding your breath whilst doing Kegels.
- Relax your legs, back, buttock and stomach muscles so that you’re just training those all-important pelvic floor muscles.
- Maintain good posture.
- If you have a prolapse, perform as many of your daily amount of your Kegel exercises in the morning as you can when your symptoms are less severe.
- Use an electronic pelvic toner to make your pelvic floor exercise sessions even more beneficial.
- Don’t give up – if you have a very weak pelvic floor, then build up gradually and be proud of each set that you do.
Sources
Choi, K. H Hong, J. Y. (2014) Korean Journal of Urology. Management of Pelvic Organ Prolapse. [online] 55(11), p 693-702. [viewed 20/03/2018]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4231145/
Farag, K. A. Uzoma, A. (2009) Obstetrics and Gynecology International. Vaginal Vault Prolapse. [online] 275621, p1-9. [viewed 21/03/2019]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2778877/
International Urogynecological Association. (2011). Recovery following vaginal repair surgery / vaginal hysterectomy. [online] International Urogynecological Association, 2011
NICE. (2015). Urinary incontinence in women: management, 1 Recommendations [online] National Institute for Health and Care Excellence, 2015 [viewed 14/03/2018]. Available from: https://www.nice.org.uk/guidance/cg171/chapter/1-Recommendations#physical-therapies
Royal College of Obstetricians and Gynaecologists. (2013). Information for you, Pelvic organ prolapse [online] Royal College of Obstetricians and Gynaecologists, 2013 [viewed 14/03/2018]. Available from: https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/gynaecology/pi-pelvic-organ-prolapse.pdf
Royal College of Obstetricians and Gynaecologists. (2018). Menopause and women's health in later life, Pelvic organ prolapse [online] Royal College of Obstetricians and Gynaecologists, 2018 [viewed 14/03/2018]. Available from: https://www.rcog.org.uk/en/patients/menopause/pelvic-organ-prolapse/



