What is the Pelvic Floor?
You might have heard of your pelvic floor muscles, also known as your Kegel or PC muscles. These all refer to the same collection of muscles, fibres and ligaments that work together to support your pelvic organs and give you urogenital control (control of both urinary and genital organs) in your pelvic floor.
The pelvic floor is made up of three main layers of muscle:
- The superficial group - This is the group of muscles that are found at the entrance to the vagina in women. They help with sexual function and help you to control the bladder. These muscles can weaken as a result of childbirth, the menopause, or gradually as you age.
- The urogenital muscle group - This is the group of muscles that surround the urinary and genital muscles, and are responsible for bladder function.
- The deep pelvic floor muscle group - These muscles are called levator ani. It extends from the pubic bone at the front, towards the coccyx at the back and the side walls towards the hips. It is a broad, thin group of muscles which is made up of 3 parts; the iliococcygeus muscle, the pubococcygeus muscle, and the puborectalis muscle.
These muscles are the main support for your pelvic floor. They stretch from your pubic bone to your coccyx, acting like a hammock to protect your pelvic organs from gravity and hold them in place. With the entries to the vagina, urethra and bowel all passing through. If you leave these muscles to weaken – as they naturally will for all of us (more quickly for mothers and those approaching menopause), you are knowingly putting yourself at risk of leaks when you laugh, cough, sneeze or even worse your pelvic floor muscles could give way completely resulting in pelvic organ prolapse.
Pelvic floor muscles are important for:
- Sexual function - In men, strong pelvic floor muscles aid erectile function and ejaculation. In women, the squeezing of the pelvic floor muscles is responsible for sexual sensation and arousal.
- Pregnancy and childbirth - In women our pelvic floor muscles provide support for the baby during pregnancy and assist in childbirth.
- Posture and support - Alongside the core muscles of the abdomen and back, the pelvic floor muscles stabilise and support the spine.
- Continence - Weak pelvic muscles can allow your bladder and rectum to drop and prolapse (bulge) into the vagina. Causing urinary and sometimes faecal incontinence where you lose control of these functions.
- Healthy bowel movements - Constipation can occur where your rectum or small bowel (small intestine) loses its support from the Kegel muscles.
Maintaining Your Pelvic Floor
The pelvic floor is not strengthened through traditional exercises such as running or sport, and as they weaken it is important that you learn how to exercise them.
You should make exercising your Kegel muscles part of your daily exercise routine. Dr Arnold Kegel published his original clinical research in 1948 about the importance of pelvic exercise – but it seems as though women still don't realise how important it really is! It's really important that you exercise the correct pelvic floor muscles in the correct way to make sure your pelvic floor is strong and healthy.
Do Men Have a Pelvic Floor?
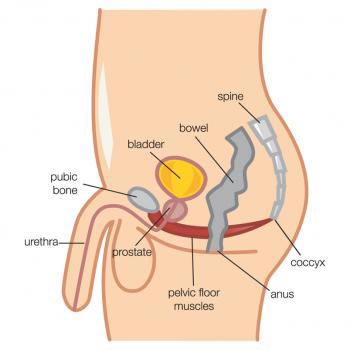
Many people don't realise that the male pelvic floor also exists and is as important as the female pelvic floor.
The male pelvic floor works in a similar way to the females as it supports the bowel and bladder, but also supports the prostate and plays a huge part in sexual function.
Sources
[3] Kegel, A. H. (1952). Ciba Clinical Symposia. Stress incontinence and genital relaxation; a nonsurgical method of increasing the tone of sphincters and their supporting structures. [online] 4(2), p 35-51 [viewed 03/04/2018]. Available from: https://pubmed.ncbi.nlm.nih.gov/14905555/
[4] Mittal, R. K. Raizada, V. (2008). Gastroenterology Clinics of North America. Pelvic Floor Anatomy and Applied Physiology. [online] 37(3), p 493-509. [viewed 03/04/2018]. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC2617789/
[5] National Childbirth Trust. (2014). Pelvic floor exercises how-to guide: Pregnancy & beyond. [online] National Childbirth Trust, 2014. [viewed 03/04/2018]. Available from: https://www.nct.org.uk/information/pregnancy/body-pregnancy/pelvic-floor-and-stomach-exercises-pregnancy
[6] NICE. (2015). Urinary incontinence in women: management, 1 Recommendations [online] National Institute for Health and Care Excellence, 2015 [viewed 03/04/2018]. Available from: https://www.nice.org.uk/guidance/cg171
[7] Rahule, A. Sagdeo, V. Soni, N. (2014). Journal of Contemporary Medicine and Dentistry. Kegel exercise in Stress Incontinence. [online] 2(3), p 20-23. [viewed 03/04/2018]. Available from: https://www.semanticscholar.org/paper/Evaluation-of-Effect-of-Kegel-Exercise-for-the-of-%2C-Soni-Rahule/20e26c8d8375900d97ab45d416870746afc85307?p2df



