Many of us will not have heard the term prolapse until we experience a problem. But what exactly is a prolapse? And why are so many of us at risk?
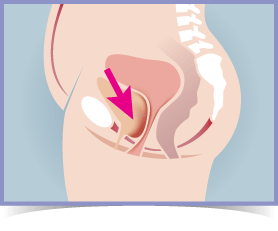
The primary cause of prolapse is weakened or damaged pelvic floor muscles. Responsible for supporting each of the pelvic organs, when they are no longer strong enough to carry out this job effectively, it can result in one or more of the organs sagging, or dropping down, into the vagina/rectum. Scarily, it is estimated that 1 in 2 women over the age of 50 will suffer with some form of prolapse [1].
There are various different types and stages which represent the prolapse severity. For some of us, the symptoms will be so mild that we won't even visit our doctor. However, even where this is the case, it can still significantly impact on our physical and emotional wellbeing.
It's therefore vital that we know the best ways to prevent and manage it!
Is it too late for me?
It's never too late to manage and in many cases even rectify prolapse
At Kegel8 we help women every day to overcome the misery that is their prolapse. What these Kegel8 users have to say is invaluable to you - if you can relate to any of the stories in our video from real Kegel8 users then act now, and manage your prolapse and live without restriction - if you can't relate to these stories yet then act now, and prevent prolapse today, before it prevents you.
What are the different types of prolapse?
If you think about it, our pelvic cavity is home to a number of extremely important organs, all of which are at risk of falling out of place. When this happens, it can affect the anterior (front) or posterior (back) wall of the vagina, and in some cases the central part of the pelvis. Different types of pelvic organ prolapse include:
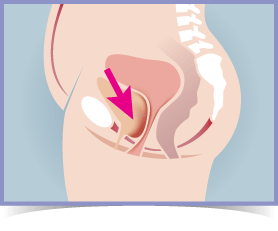
Cystocele Prolapse
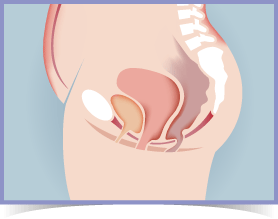
Rectocele Prolapse
Cystocele - A prolapsed bladder. The most prevalent form of prolapse; this is where the bladder drops downwards into the vagina.
More Info >
Cystourethrocele - Both the urethra and bladder prolapse at the same time. It is quite common for this to happen.
Rectal Prolapse - Complete rectal prolapse. This occurs when the rectum protrudes out of the body through the anus.
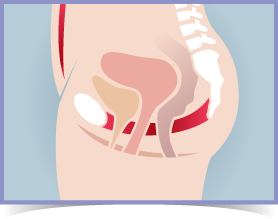
Uterine Prolapse - Prolapse of the uterus (womb) into the vagina. Those who suffer with a prolapsed uterus are at a greater risk of developing another form of prolapse.
More Info >
Urethrocele - The tissues surrounding the urethra descend into the vagina.Rectocele - Partially prolapsed rectum. The front wall of the rectum bulges into the vagina. Those with rectocele are more prone to developing cystocele.
More Info >
Enterocele - The small bowel drops against and moves the upper wall of the vagina, causing it to descend into the gap between the rectum and the vagina.
More Info >
Vaginal Vault - This only occurs in women who have undergone a hysterectomy. The closed end of the vagina collapses in on itself, dropping down into the vaginal canal or outside the vagina.
More Info >
What causes prolapse?
"Research tells us that up to 50% of women who have had children will suffer from prolapse in their lifetime."
Sue Croft - Physiotherapist & Author

It's the age-old question: "Why me?"
You've taken good care of yourself over the years, maintaining a healthy diet and doing the obligatory 30 minutes of exercise daily. So why are you still at risk of developing prolapse?
Well, you may be surprised to learn that this alone is not enough to keep your pelvic floor muscles strong and healthy. When they are weak, they are unable to support the pelvic organs effectively. This may occur for a number of different reasons, including:
Childbirth
Increased pressure in the abdomen
Coughs, constipation, weight
Age
Gynaecological Surgery
Menopause
Congenital Disorders
Hysterectomy
What are the symptoms of prolapse?
Have things been becoming a bit of a drag recently? Or are you simply losing your sense of humour when it comes to those laughter leaks?
Well, there really is nothing funny about prolapse, and it's entirely possible that you could have suffered one without even realising. Prolapse symptoms vary depending upon the stage it is at, however, common indications include:
- A 'dragging' sensation in the vagina or lower back
- Pelvic and/or abdominal pain
- A lump inside or outside the vagina
- Struggling to empty the bowel
- Dyspareunia (painful sex) or lack of intimate sensation
- Urinary abnormalities such as a slow stream, incomplete emptying of your bladder, urinary frequency/urgency or stress incontinence
What are the treatments for prolapse?
It can be a devastating blow to learn that you have suffered a prolapse. Indeed, living with the symptoms is certain to take its toll, both physically and emotionally. Inspiring feelings of inadequacy and self-consciousness, many times the result is anxiety or depression. This alone can have a significant impact on day-to-day life.
Worried there's nothing you can do? Well fear not, there are several different ways to treat prolapse, which vary largely depending upon the severity of it. Minor prolapse can be treated by making simple lifestyle changes; whereas more severe forms may require surgery. Pelvic floor exercise is recommended as a viable treatment option for everyone, as not only will it rebuild strength, it could also alleviate the associated symptoms and prevent the prolapse from worsening. Different types of treatments include:
Lifestyle changes
All the motivation required to shift those few extra pounds. Achieving a healthy weight will strengthen the pelvic floor and prevent your prolapse from worsening. Avoid heavy lifting and activities that put undue pressure on the abdomen.
Pelvic floor exercise
An effective way to prevent, manage and treat prolapse. Much like any other work out, pelvic floor exercise will increase tone and strength in the muscles over time. This will help to 'lift up' the prolapsed organs.
Pessary
Typically used to treat uterine prolapse; a pessary is often employed as a temporary solution for pregnant women, women who have given birth, or those awaiting surgery. In rare cases, it will be offered as a permanent solution for those of us who do not wish to have, or are unsuitable for, surgery. Side effects may include bleeding and bladder weakness.
Hormone Replacement Therapy (HRT)
This is sometimes offered where prolapse is attributed to the menopause. Increasing the level of oestrogen with the use of HRT may rebuild muscle strength, alleviating the symptoms and preventing the prolapse from worsening. A GP can explain the different types of HRT available and help you choose one that's suitable for you. In the UK women will only need to pay one prescription charge for up to a year's supply of HRT medication.
Surgery
In cases where prolapse is extremely severe, surgery could be the best and, indeed, the only option. However, all too often we opt for surgery without being fully aware of our choices. Surgery may involve the insertion of synthetic mesh, vaginal wall repair or suspension of the prolapsed organ. In more serious cases, a hysterectomy or obliterate surgery may be performed.
It is important to explore all other options before committing to this type of treatment, because as with any kind of procedure, prolapse surgery carries with it some degree of risk. Side effects can range from bleeding/infection, constipation, damage to neighbouring organs, painful sex and problems with passing urine. Additionally, approximately 1/3 of women who have prolapse surgery may need more than one operation as there is a 25-30% chance that it could return, or a different type of prolapse could develop [2].
In some cases, surgery may repair pelvic prolapse, but not alleviate associated symptoms.
It's true; the importance of regular exercise has been instilled in us from an early age. However, despite this, many of us remain unaware that it doesn't end with a quick visit to the gym, or a brief burst of cardio now and then. In fact, too many of us still associate the need for exercise with outwardly appearance. But shouldn't exercise be about health, rather than vanity?
Our pelvic floor has an extremely important role within the body; it maintains the everyday functioning of the bladder and bowel, while supporting all of the pelvic organs. It is therefore vital that it is strong enough to do so.
So, how do we increase the strength of our pelvic floor? Well, as with any muscle group; exercise it and it becomes stronger. A strong pelvic floor will be more equipped to hold the organs in place, thus reducing the risk of prolapse. Strengthening the pelvic floor can also improve an existing prolapse and alleviate the associated symptoms as it springs back into place.
So, why not exercise the muscles that matter? After all; it's what's on the inside that counts!
Alleviate the symptoms of pelvic organ prolapse & strengthen the pelvic floor in just 12 weeks, with the help of the Kegel8 Ultra 20 & Amanda Savage!

Amanda Savage is one of the UK’s leading specialist pelvic floor and women’s health physiotherapists, who has worked in the field for over 20 years offering supervised pelvic floor muscle training and support for the recovery of pelvic organ prolapses, incontinence and pelvic surgeries. With post-graduate qualifications, including a master’s degree from the University of Cambridge, she has also gained full membership of the Professional Network of Pelvic, Obstetric & Gynaecological Physiotherapy (POGP). As a Kegel8 ambassador, Amanda Savage has worked alongside us for many years in the development of our best-selling device, the Kegel8 Ultra 20 V2 Electronic Pelvic Toner, to ensure its efficacy. In addition, she has been integral to ensuring all supporting information and instructions are medically accurate so that the device is used correctly/effectively, and treatment is tailored to the specific condition of the user.
Find out more about Amanda Savage, her qualifications, experience, knowledge, and affiliations here.
Comes complete with an easy exercise plan, created by Amanda Savage, to get results in 12 weeks!
Here at Kegel8, we are all too aware of the discomfort, not to mention the anxiety, that is caused by pelvic organ prolapse. So, if you are experiencing an uncomfortable ‘dragging’ sensation, are struggling with bladder and bowel control, bowel emptying and a lack of intimate sensation, you are certainly not alone! Indeed, more common that you may realise, pelvic organ prolapse affects millions of people worldwide. And we are extremely familiar with the impact it has on both physical and emotional well-being, as well as on life in general.
It’s true that, left untreated, the symptoms of pelvic organ prolapse will simply worsen over time. However, they should by no means be accepted as an inevitability! Indeed, regular pelvic floor exercise has been proven to build muscle and tone, creating a thicker support shelf for the organs to rest on. This essentially holds them up and keeps them in place. In addition, much like any other exercise, it builds strength and tone to ensure the muscles do not tire easily and can react quickly to provide additional support during strenuous activities. This improved endurance and strength also helps with bladder and bowel control. So, by simply performing regular pelvic floor exercise, you can get your life back on track!
The included easy exercise plan was created by Amanda Savage to prevent, treat, and alleviate the associated symptoms of pelvic organ prolapse. It is proven to build muscle and tone and create a thicker support shelf for the organs to rest on, essentially holding them up and keeping them in place. In addition, this simple exercise regime will improve endurance and ensure the muscles do not tire as easily, so that they can react quickly and provide the optimum support when performing strenuous activities. This improved endurance and strength also helps with bladder and bowel control and the contractions have been shown to calm the nerves responsible for a sensitive bladder. The plan even encourages the user to practise contracting their muscles alongside the machine, which prepares them for ‘real life’ scenarios when they don’t have access to the machine.
So, why opt for an electronic pelvic floor exerciser rather than performing your Kegels independently?
It is thought that many women push downwards when performing independent pelvic floor exercises, which, rather than strengthening the muscles, can lead to further damage. In addition, it can be difficult to locate and target the correct muscles, making exercise less effective. The Kegel8 Ultra 20 V2 Electronic Pelvic Toner removes the guesswork and essentially acts as a Sat-Nav for your pelvic floor muscles, correctly targeting and stimulating a contraction within them using a small electric current. These contractions build strength and tone in a matter of weeks! With 20 clinically proven pelvic floor exercise programmes which vary in frequency, intensity and duration, the Ultra 20 is proven to treat a variety of different conditions, including pelvic organ prolapse and bladder/bowel control and emptying. And, in addition to tailored programmes, the specific 12-week exercise plans created by Amanda Savage advise exactly how the device should be used, depending upon the condition, to ensure the very best treatment.
So, why opt for an electronic pelvic floor exerciser rather than performing your Kegels independently?
It is thought that many women push downwards when performing independent pelvic floor exercises, which, rather than strengthening the muscles, can lead to further damage. In addition, it can be difficult to locate and target the correct muscles, making exercise less effective. The Kegel8 Ultra 20 V2 Electronic Pelvic Toner removes the guesswork and essentially acts as a Sat-Nav for your pelvic floor muscles, correctly targeting and stimulating a contraction within them using a small electric current. These contractions build strength and tone in a matter of weeks! With 20 clinically proven pelvic floor exercise programmes which vary in frequency, intensity and duration, the Ultra 20 is proven to treat a variety of different conditions, including pelvic organ prolapse and bladder/bowel control and emptying. And, in addition to tailored programmes, the specific 12-week exercise plans created by Amanda Savage advise exactly how the device should be used, depending upon the condition, to ensure the very best treatment.
We are here to help you before and during your purchase. Whether you need help selecting the right pelvic floor toner, have a question about one of our Kegel8 units or are still unsure whether this is the right product for you. We want to help you make sure you have the right device for your individual needs and that you can achieve results that last.
References
Hagen S, Stark D Conservative prevention and management of pelvic organ prolapse in women (review).
Available from: http://www.cqc.org.uk/sites/default/files/media/documents/101006_mat10_historical_comparisons_tables_final.pdf
Bladderandbowelfoundation.org,(2014). Prolapse Treatments - Bladder and Bowel Foundation. [online] John Hopkins University Press, 2012 [Accessed 4 Aug. 2014].
Available from: http://www.bladderandbowelfoundation.org/bladder/bladder-problems/prolapse-treatments.asp
Johns Hopkins University Press Blog, (2012). The Doctor Is In: Women's pelvic health, fact or fiction?. [online]
Available at: http://jhupressblog.com/2012/10/09/the-doctor-is-in-womens-pelvic-health-fact-or-fiction/ [Accessed 11 Jun. 2014].