We've all seen footballers fall to the ground in agony from a seemingly minor injury, but is there more to it than meets the eye?
The hips and pelvis of a professional footballer are put under a lot of stress during practices and games. Football requires a lot of pivoting, rapid acceleration and deceleration, and, of course, kicking.
The following injuries are common in both professional and amateur footballers, and can mean the end of a sports career and debilitating pelvic pain.
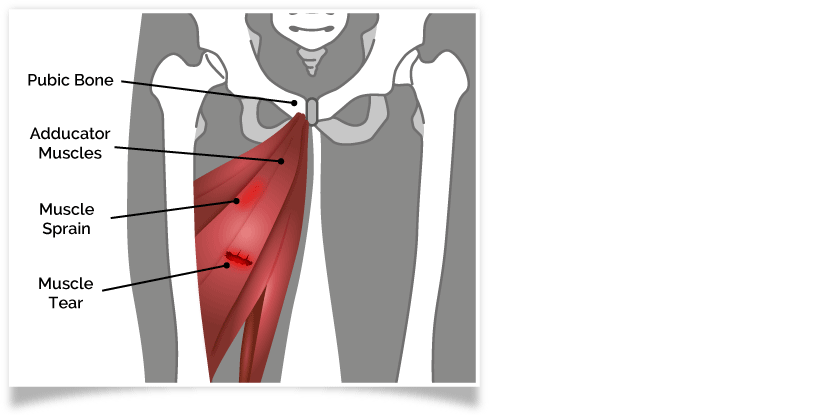
Groin Strains
The adductor muscles of the inner thigh connect the femur thigh bone to the pubic bone. When a footballer kicks, these muscles lengthen as the leg moves up. When kicking repetitively, this can strain the muscle. The added rapid acceleration and deceleration of the footballer adds extra strain, and after many kicks, the muscles can eventually tear.
This injury is called a groin strain and accounts for just under 5% of sport related injuries.
Osteitis Pubis
Each time a footballer kicks, the pelvis twists. This repeatedly stresses the joint between the two sides of the pelvis - the pubic symphysis joint. This joint can become inflamed which causes a condition called osteitis pubis.
The inflammation can spread to the surrounding muscle, leading to pain in the adductor muscles of the inner thigh, and the abdominal muscles, as well as the original concentration of pain in the pelvis. Kicking more on one side can cause a muscle imbalance between the hips and abdomen, which can further inflame the injury.
Osteitis pubis accounts for 5% of all footballers injuries.

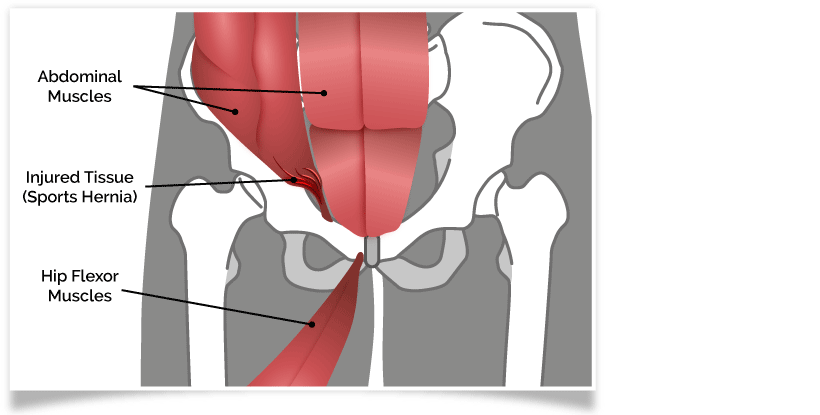
Athletic Pubalgia
Another condition caused by kicking, pivoting on the spot and quick acceleration and deceleration, is athletic pubalgia. The twisting motion damages the tendons which connect the oblique muscles, of the lower abdomen, to the pubic bone. The tendons can separate from the bone, leading to pelvic floor weakness. This is a soft tissue injury of the muscles in the lower abdomen and groin, and is often felt on one side of the pelvis more than the other.
NB: Athletic pubalgia is often incorrectly called 'sports hernia' in the press.
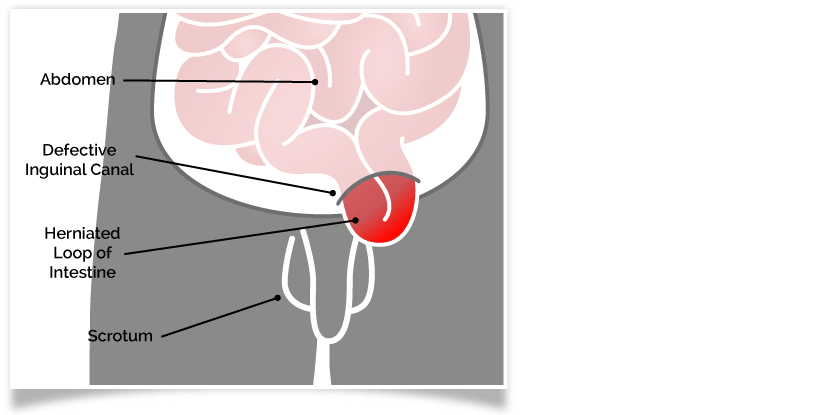
Groin Hernias
Hernias are not exclusive to exercise. They can occur when you lift a heavy object, or strain as a result of constipation.
Groin hernias, however, are very common in footballers. They occur where there is a weak spot in the abdominal muscles. The footballer will feel general groin pain for a long time before the hernia occurs. If the footballer continues to participate in exercise regardless of this pain, one of the pelvic organs or pelvic tissue, can come through the muscle layer and protrude painfully under the skin as a hernia.
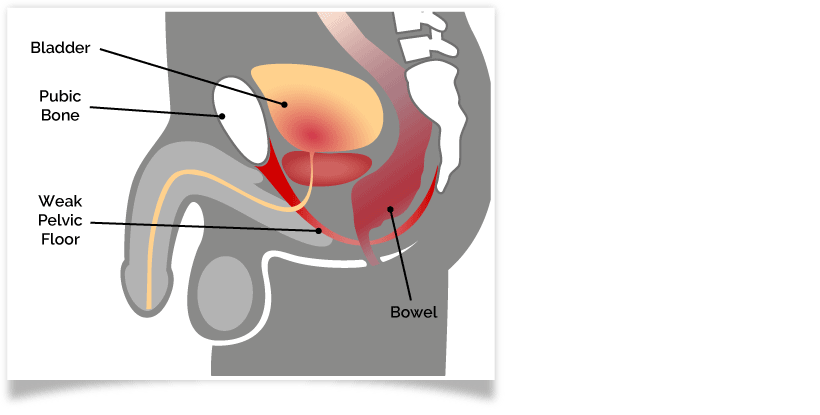
Pelvic Floor Damage
The pelvic floor experiences a considerable amount of damage during high impact exercises. These are any exercise where both feet are off the ground at points, or land heavily on the ground in turn.
When both feet land back on the ground, pressure shoots up the legs to the pelvis, injuring the pelvic floor.
It's Not All Bad News for Footballers
Regular exercise is essential for good cardiovascular health and maintaining strength. However, its important to rest often and allow your body to recover before exercising again. If you feel pain during or following exercise, which you do not easily recover from, consider:

- Creatine and protein supplementation - To help your muscles recover from damage quicker and build muscle tone.
- Taking Vitamin D - Vitamin D improves general musculoskeletal health. It slows the skeletons natural ageing and reduces the rate of fractures as we get older.
- Increasing rest periods - Giving your body time to recover.
- Exercising to strengthen your core - Having a strong core can prevent muscle imbalances and provide better support for your posture.
- Introducing stretching exercises and yoga into your exercise programme - To strengthen the muscles, improve flexibility and avoid muscle stiffness. Particularly of the adductor muscles in the inner thigh.
Sources
[1] Angoules, A. G. (2015). World Journal of Orthopedics. Osteitis pubis in elite athletes: Diagnostic and therapeutic approach. [online] 6(9), p672-679. [viewed 30/05/18]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4610909/
[2] Brown, A. Abrahams, S. Remedios, D. Chadwick, S. J. (2013). British Journal of General Practice. Sports hernia: a clinical update. [online] 63(608). [viewed 30/05/18]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3582984/
[3] Ellsworth, A. A. Zoland, M. P. Tyler, T. F. (2014). International Journal of Sports Physical Therapy. Athletic Pubalgia And Associated Rehabilitation. [online] 9(6), p774-784. [viewed 18/06/18]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4223287/
[4] Liberi, V. Liberi , K. H. (2011). Human Kinetics. Pelvic Pain and Pelvic Floor Dysfunction in Male Athletes. [online] 16(1), p8-12. [viewed 09/05/18]. Available from: https://journals.humankinetics.com/doi/abs/10.1123/ijatt.16.1.8?journalCode=ijatt
[5] Larson, C. M. (2014). Sports Health. Sports Hernia/Athletic Pubalgia. [online] 6(2), p139-144. [viewed 20/06/18]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3931344/
[6] Nygaard, I. E. Shaw, J. M. (2016). American Journal of Obstetrics and Gynecology. Physical Activity and the Pelvic Floor. [online] 214(2), p164-171. [viewed 30/05/18]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4744534/
[7] Rodriguez, C. Miguel, A. Lima, H. Heinrichs, K. (2001). Journal of Athletic Training. Osteitis Pubis Syndrome in the Professional Soccer Athlete: A Case Report. [online] 36(4), p437-440. [viewed 15/06/18]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC155442/
[8] Sedaghati, P. Alizadeh, M-H. Shirzad, E. Ardjmand, A. (2013). Trauma Monthly.Review of Sport-Induced Groin Injuries. [online] 18(3), p107-112. [viewed 18/06/18]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3864393/
[9] Haines, S. T. Park, S. K. (2012). Pharmacotherapy. Vitamin D supplementation: what's known, what to do, and what's needed. [online] 32(4), p354-382 [viewed 18/06/18]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/22461123




