Prolapse Surgery
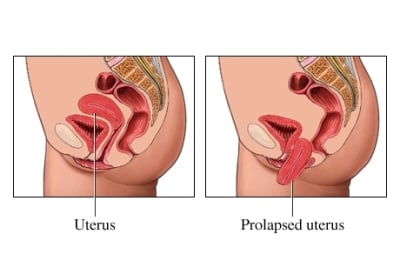
While not always the case, it’s not uncommon for women to experience pelvic organ prolapse after pregnancy and childbirth. This occurs when one of your pelvic organs ‘drops’ because it is no longer held in the correct position.
Although this can be rather distressing to experience, there are a variety of prolapse surgery and non-surgical solutions out there that have proven to be successful in minimising and reversing the effects of pelvic prolapses.
Why might you need pelvic floor surgery?
Whether you experienced a difficult pregnancy or a long birth, there’s no way to tell which, if any of your pelvic organs, has the potential to prolapse. However, common prolapsed organs usually include:
- bladder prolapse(cystocele)
- Urethral prolapse
- uterine (womb) prolapse
- Vaginal vault prolapse
- bowel prolapse (enterocele)
- rectal prolapse (rectocele)
Regardless, any prolapsed organ may require surgery to return it to its normal position and give it the support it needs to steady itself. But, with that being said, it’s up to your surgeon to decide if an operation is required.
And, naturally, if your surgeon does decide that surgery is the best option, then we want to make sure that you know all about the prolapse repair process, as well as life after prolapse surgery so that you can have a swift recovery.
What are the different types of prolapse surgery?
- Vaginal Repair: In a large majority of cases, prolapse surgery often involves vaginal repair due to another prolapsed organ pushing against your vagina. This may include a vaginal hysterectomy where your uterus is removed via the vagina. This won’t leave a scar as all the stitches are internal. Once this has been done, your surgeon will often use a mesh (TVT) to help support your vagina and prevent further prolapse.
- Posterior Intravaginal Sling Plasty: Sometimes, you may suffer vaginal prolapse after a hysterectomy. To treat this, your surgeon will place a mesh inside the vagina to ‘anchor’ it and help to support the vagina.
- Sacrospinous Fixation: To support the vagina, sometimes surgeons will place one or two very deep internal stitches inside you. These stitches go into a strong ligament in your pelvis, called the sacrospinous ligament, with the aim of helping to prevent your prolapse from coming back.
- Sacrocolpoplexy: If you have a particularly severe or complicated prolapse, surgeons may perform this type of operation. Your surgeons will make a cut across your abdomen, to fix the vagina to the bone to the back of your pelvis. This will then be supported by a mesh to give stronger support and help to hold things in place.
Of course, if another organ is prolapsed alongside your vagina, then your surgeon will almost certainly have to carry out a more complex procedure to rectify the problem. Take a look at our guides on the topic to learn more about prolapsed bladder surgery and neobladder surgery, for example.
What are the risks of prolapse surgery?
As with any surgery, there are risks associated with prolapse repair that may require further surgery to fix:
- TVT mesh erosion: With prolapse surgery, there is the risk that the mesh used to support your internal organs can erode or become infected. This is a small risk but it may require further surgery to remove the mesh or repair it.
- Further prolapse: Studies show that about a third of women who undergo prolapse surgery end up having further surgery for a later prolapse. This is because there is a strong link between initial and later prolapses, though not with the surgery to repair them. Essentially, if a woman has had one prolapse, it is possible that she may get another. That is why it is so important to strengthen the pelvic floor both before and after surgery.
- Not all symptoms may improve: Many women find that, although they no longer have the ‘bulging’ or ‘dragging’ associated with prolapse after surgery, they still may suffer from incontinence or constipation because prolapse surgery only treats the symptoms, not the underlying cause of prolapse. Again, it is vitally important to strengthen the pelvic floor, not only to prevent your prolapse from recurring but to help treat the incontinence symptoms too.
Are there any non-surgical prolapse surgery options?
While surgery is often the most common way to repair a prolapse, it’s not the only option.
For example, a very mild prolapse could be fixed through more conservative treatment options, including pelvic floor exercise (which we of course recommend strongly regardless of whether or not you have experienced a prolapse) and the use of a vaginal pessary.
However, we still suggest seeing a doctor should you experience any prolapse symptoms in order to catch a potential prolapse as soon as possible.
Life after prolapse surgery
As with all surgery, bed rest and self-care vital after prolapse surgery if you want to ensure a full recovery. Ask your surgeon for advice on what to do in the weeks and months after your operation and follow this to the letter.
On top of this, strengthening your pelvic floor muscles before and after prolapse surgery with a pelvic floor toner will greatly improve your surgical outcome and help you avoid further prolapse surgery in the future.
Indeed, after prolapse surgery with or without pelvic floor repair, it’s vitally important to Kegel exercise, as this will give you the best possible surgical outcomes. You can do the 'manual' squeeze and lift exercises or you can invest in a pelvic floor toner to automatically strengthen and tone your pelvic floor.
Also, it’s important to remember that you should not use electronic stimulation for around 3 months after surgery or until your surgeon gives the all-clear that it’s safe to use. Remember, Kegel8 are here to help you, so if you need any advice on how a Kegel8 pelvic toner can help with prolapse, please call us – we’re always happy to help.



