There are a great number of conditions that can lead to pelvic pain, whether acute or chronic. If you are suffering from pelvic pain, it's important to see a doctor so that you can discover the underlying cause.

Adenomyosis
Adenomyosis is a condition where endometrial tissue (the tissue that normally lines the uterus) grows into the wall of the uterus. This is different from endometrosis, because the tissue does not grow outside the uterus, rather inside.
Read More
Adenomyosis normally affects women after childbearing age, but it can affect all women, and the pain felt can be very intense. Some women who suffer adenomyosis say that the pain is not only confined to the pelvic area but spreads into the legs. It can lead to very heavy periods (menorrhagia) and can cause fertility problems such as difficulty conceiving and greater risk of miscarriage.
Treatment for adenomyosis normally includes hormone therapy and painkillers. The standard surgical adenomyosis treatment is hysterectomy.

Endometriosis
Endometriosis is a relatively common condition where cells like the ones found in the lining of the womb grow outside of the womb on other organs such as your ovaries, fallopian tubes and bladder. Like the cells inside of your womb, these will break down every month during your period, but can cause a great deal of pain because the blood has nowhere to go.
Read More
Endometriosis can cause chronic pelvic pain, and lots of women describe it as being like constant period pain. Endometriosis can cause very heavy periods and can lead to fertility problems such as increased risk of miscarriage and difficulty getting pregnant. Doctors aren't 100% sure what causes endometrosis, but it's more common if your mum or sister has it too, which suggests it could be inherited, and women who started their period early and those who had frequent heavy periods can be more at risk.
Treatment for endometriosis includes hormone treatments, painkillers and surgery, including laporoscopy and hysterectomy.
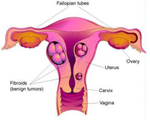
Fibroids
Fibroids are non-cancerous growths, or tumours, that grow in and around the womb (uterus). Fibroids are very common, and most women don't even know that they have them, however they can cause heavy periods (menorrhagia) and pelvic pain.
Read More
If fibroids become particularly large, they can cause a great deal of pain in the pelvic area, and may make sexual intercourse uncomfortable. Unless fibroids are causing problems, no treatment is usually necessary, however if fibroids are causing pain and discomfort, doctors may provide medication such as hormone treatments to reduce heavy periods, painkillers and fibroid surgery which involves removing either just the fibroids themselves, or removing the whole uterus as part of a hysterectomy.

IBS (Irritable Bowel Syndrome)
IBS, or Irritable Bowel Syndrome is very common, and affects up to 1 in 5 people at some point in their lives. IBS causes painful cramps, diarrhoea, constipation and bloating, and can cause chronic pelvic pain if it goes on for a long time. IBS is often linked to certain foods and stress, but it can be managed.
Read More
The key to managing IBS often lies in diet – GPs often recommend that you keep a food diary to see if there are particular foods that trigger IBS symptoms. It's also recommended to eat little and often and to not rush food. Stress is often one of the biggest IBS triggers, so learning relaxation techniques such as breathing exercises, yoga and regular gentle exercise can help keep IBS symptoms under control.
There are medications that can be given to help deal with the symptoms of IBS, these include laxatives for people who suffer IBS with constipation, antimotility medication to help with diarrhoea and antispasmodic medication to help treat stomach cramps.
IBS can be really damaging to your pelvic floor, so it's important not to strain to go to the toilet – if you suffer from constipation, try using a Squatty Potty (available from our friends at StressNoMore.co.uk).
Ovarian Cysts
Ovarian cysts are very common, and many women have them and never know anything about it. However, if the cysts get bigger, or depending on the type of ovarian cyst, it may cause stomach pain, pelvic pain and bloating.
Read More
There are different types of ovarian cyst – and don't panic, an ovarian cyst is only very rarely ovarian cancer. Follicular cysts and corpus luteal cysts form during your menstrual cycle when the egg doesn't leave the ovary properly – if you have one of these cysts, it will usually go away by itself within a few months and you probably won't even know you have it. You can also get growths of cells on the ovary and these are called ovarian tumours. Most of the time they are benign and harmless, but very rarely can be cancerous, so if you think you have an ovarian cyst, it's worth seeing your doctor just to be checked out.

Pelvic Abscess
Pelvic abscesses are rare and can sometimes occur if you've had an infection in your pelvic area, for example if you've had appendicitis or an operation. If you've got a pelvic abscess, you will feel poorly with it, you'll have a fever and a lot of pelvic pain. If you have a pelvic abscess, you will need an operation to clear it up.
Read More
If you've had an operation or an infection in your pelvic area and start to feel ill afterwards, it's important to see your doctor if you think you have a pelvic abscess. If a pelvic abscess isn't treated, it can cause widespread damage and make you very ill. Pelvic abscess treatment involves an operation to drain the abscess, then doctors will put a tube into your stomach so that the abscess can keep on draining.

Pelvic Congestion
Pelvic congestion is the name given to varicose veins in the stomach. This can cause chronic pelvic pain, and just like the pain from varicose veins in the legs, it gets worse after lots of standing, and the pain goes away when the sufferer lies down.
Read More
Pelvic Congestion treatment involves painkillers and hormone therapy to make the ovaries work less quickly. The only full treatment for pelvic congestion involves surgery to take away the varicose veins. Pelvic pain caused by pelvic congestion is usually a dull and aching pain.

Pelvic Inflammatory Disease
Pelvic Inflammatory Disease or PID is an infection that affects the womb, ovaries and fallopian tubes. It's very common but can cause a great deal of pelvic pain and discomfort, and painful intercourse, as well as discharge and fever.
Read More
PID mainly affects women between the ages of 16-24 and is most common in sexually active women. If you think you might have PID, it's important to see your GP, because left untreated, it can eventually cause infertility. If you have had chlamydia, gonorrhoea or another sexually transmitted disease, it's important to keep an eye out for the signs of PID afterwards. You can prevent PID by using condoms. PID causes inflammation and infection of the womb, fallopian tubes and abscesses, so it's important to get checked if you think you might have pelvic inflammatory disease.

Prolapse
Prolapse is the name given to when one or more of your organs slips out of place. It can cause a heavy, dragging feeling and be really uncomfortable, especially if you have been walking around or have been on your feet all day. A Kegel8 Ultra Pelvic Toner can help with prolapse.
Read More
Prolapse can be uncomfortable and distressing, but it's a lot more common than you may think. It's estimated that 50% of women over 50 will suffer some form of pelvic organ prolapse in their life. If you have one prolapse, for example a rectocele or rectal prolapse, it's more likely that you will suffer another prolapse, for example a cystocele or bladder prolapse, so it's really important to strengthen your pelvic floor if you have prolapse or think you may be at risk of prolapse. By strengthening the pelvic floor, the muscles can better support your pelvic organs and can reduce the pelvic pain and everyday symptoms of prolapse to make your life much easier.
Urinary Tract Infection
A urinary tract infection or UTI is a very common cause of pelvic pain and discomfort in the lower abdomen. As well as this, you may feel burning or pain when you urinate, you may need to go for a wee more often, or you may feel generally unwell.
Read More
Urinary tract infections are common and easily treatable. They can affect men and women of all ages but are more common in women. They usually pass within a few days, and you can take cystitis powder to make your wee less acidic so it will burn less. They can also be treated with a short course of antibiotics.
How Can Kegel8 Pelvic Toners Help With Chronic Pelvic Pain Syndrome?
- Kegel8 Ultra 20 will help to stimulate blood flow and improve circulation with the pelvic area.
- By using Tibial Nerve Stimulation or Sacral Nerve Stimulation you can treat outside the body without a probe - this is particularly useful where chronic pain is present and you do not want to, or are unable to insert a vaginal or anal electrode probe.
- Kegel8 fights pain and helps to relax a tense, in-pain pelvic floor, and automatically perfroms pelvic exercises to improve strength and control.
Read More:
- What else can you do to make your kegel exercises even more effective and get a stronger pelvic floor faster?
- Kegel8 Pelvic Toners can help to improve Sexual Intimacy for you both.
- See the UK's best pelvic floor exercise machine the Kegel8 Ultra 20 Pelvic Toner - it can help with Chronic Pelvic Pain Syndrome and help you get your pelvic floor strong again.
- Learn how sacral nerve stimulation can help with chronic pelvic pain syndrome
- Tibial Nerve Stimulation - amazing new treatment for pelvic pain, incontinence and pelvic floor weakness - without inserting a probe!




