Age. Weight. Exercise. These are all known risk factors for developing a pelvic floor disorder. But, would it ever cross your mind that the colour of your skin can determine your likelihood of developing incontinence, or pelvic organ prolapse? Read on to discover how your race can affect the development of a pelvic floor disorder.
How Does Race Affect Incontinence?
Urinary incontinence is the unintentional passing of urine. Not only can it be inconvenient, but it can also cause embarrassment and can stop you from enjoying social activities. Incontinence can be affected by numerous factors; age, weight, fitness, but did you know that it can also be affected by race and ethnicity? A study from the University of California identified that race can affect the frequency, type, and severity of incontinence in different ways.
Types of Incontinence
- Stress Incontinence - Hispanic and White women are the most likely to suffer from stress urinary incontinence, whereas Black women are the least likely to suffer.
- Urge Incontinence - Urge incontinence is more likely to occur in Black women, and least likely to occur in Asian-American women.
- Mixed Incontinence - Hispanic women are also the most likely to suffer from both stress and urge incontinence. Luckily, Black women are the least likely to suffer from mixed incontinence.
Incontinence Severity
Hispanic women are the most likely to suffer from both moderate and severe incontinence. Whereas Asian-American women have the least risk of developing either moderate or severe incontinence.
Some studies suggest that black women are more likely to have higher risk factors for urge incontinence, including obesity, diabetes, smoking and hysterectomy. Other studies have reported that black women have higher urethral closure pressure, volume and length, as well as stronger pelvic muscle strength; also suggesting a reason as to why they may be least likely to suffer with stress incontinence.
How Does Race Affect Prolapse?
If your pelvic floor muscles become weak, one or more of your pelvic organs can droop down from their normally elevated position and bulge into the vagina or rectum. Prolapse is a common condition and thought to affect over 40% of women over 50 years of age. However, although healthy pelvic floor muscles are a vital way of preventing prolapse, there are some risk factors that can’t be altered.
Your race can impact upon the development of pelvic organ prolapse. White women are far more likely to develop pelvic organ prolapse than African-American women. In fact, White women undergo surgery for prolapse 3x more than African-American women.
This could be caused by differences in our collagen levels. White women begin to lose collagen earlier than Asian, Hispanic and African-American women, resulting in an earlier loss of skin firmness and elasticity. An increased collagen production in African-American women results in skin that maintains its structural integrity and youthful appearance for longer than those of lighter skin types. This could also explain why after vaginal childbirth, white women demonstrate less pelvic floor mobility than African-American women.
How Does Race Affect Pelvic Pain?
Pelvic pain can be caused by a variety of pelvic problems, such as uterine fibroids and endometriosis. Non-cancerous growths that develop in or around the uterus are known as uterine fibroids, and endometriosis is a condition where the tissue that lines the womb is found outside of the womb. These can both cause uncomfortable pain in your lower stomach and back and can prevent you from engaging in sexual activity.
Both of these pelvic conditions can be affected by your race. Uterine fibroids are known to be more common in African-American women; African-American women are more likely to be predisposed to larger and more symptomatic non-cancerous growths in or around the womb. Whilst endometriosis is more commonly found in White women.
A 2007 study from the University of Southern California found that compared with white women, womb cancer rates are 24% lower in African-American women, 39% lower in Japanese Americans, and 37% lower in Hispanic women.
Preventing and Treating Pelvic Floor Disorders
Maintaining and improving your pelvic floor can be achieved through one simple activity – Kegels. Pelvic floor exercises can help to both prevent and treat a wide variety of pelvic floor disorders, including incontinence, prolapse and pelvic pain.
If you’re not sure whether you’re performing Kegels correctly, try using a biofeedback device to help guide you through your pelvic floor exercises correctly and effectively. Alternatively, you can use an electronic pelvic toner to locate and exercise weak pelvic floor muscles for you. The Kegel8 Ultra 20 Electronic Pelvic Toner has 20 clinically-proven pelvic floor exercise and relaxation programmes to help you improve a range of pelvic floor issues.
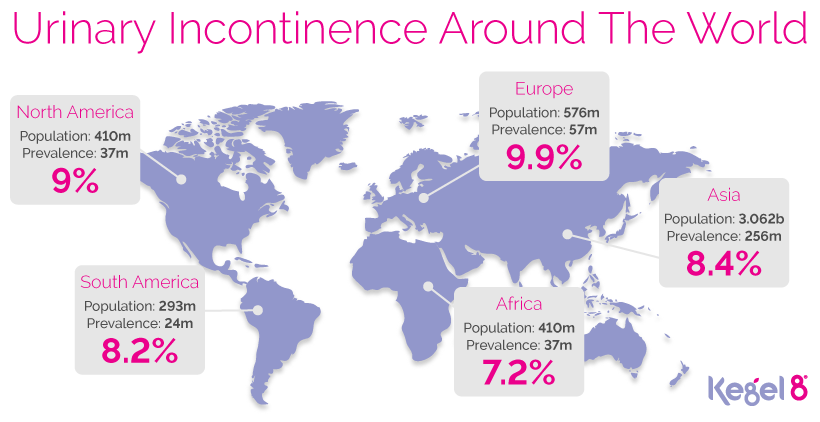
To improve quality of life for all women living with pelvic floor disorders, it’s important to recognise that urinary incontinence prevalence differs by race. Help spread awareness of how race can impact on incontinence today!
Sources
[1] Allanda (2017) Incontinence Statistics [online]. Allanda [viewed 08/10/2018]. Available from https://www.allaboutincontinence.co.uk/incontinence-statistics
[2] Brissett AE, Naylor MC. The aging African-American face. Facial Plast Surg. 2010;26(2):154–163.
[3] Continence Foundation of Australia (2018) Urge Incontinence [online]. Continence Foundation of Australia [viewed 08/10/2018]. Available from https://www.continence.org.au/pages/urge-incontinence.html
[4] Handa, V.L., Lockhart, M.E., Fielding, J.R., Bradley, C.S., Brubakery, L., Cundiffy, G.W., Ye, W., Richter, H.E. (2008) Racial Differences in Pelvic Anatomy by Magnetic Resonance Imaging. Journal of Obstetrics and Gynecology. 111(4), pp. 914-920.
[5] Hendrix, S.L., Clark, A., Nygaard, I., Aragaki, A., Barnabei, V., McTiernan, A. (2002) Pelvic organ prolapse in the Women’s Health Initiative: gravity and gravidity. American Journal of Obstetrics and Gynecology. 186, pp. 1160–1166.
[6] Irwin et al. (2011) BJU Int. 108(7), pp. 1132-1138.
[7] Jacoby, V.L., Fujimoto, V.Y., Giudice, L.C., Kuppermann, M., Washington, A.E. (2010) Racial and Ethnic Disparities in Benign Gynecologic Conditions and Associated Surgeries. American Journal of Obstetrics and Gynecology. 202, pp. 514-521.
[8] Luber, K.M., Boero, S., Choe, J.Y. (2001) The demographics of pelvic floor disorders: current observations and future projections. American Journal of Obstetrics and Gynecology. 184, pp. 1496-1501.
[9] Mayo Clinic (2017) Stress Incontinence [online]. Mayo Clinic [viewed 08/10/2018]. Available from https://www.mayoclinic.org/diseases-conditions/stress-incontinence/symptoms-causes/syc-20355727
[10] National Association for Continence (2018) Mixed Incontinence [online]. NAFC [viewed 08/10/2018]. Available from https://www.nafc.org/mixed-incontinence/
[11] NHS (2015) Endometriosis [online]. NHS [viewed 08/10/2018]. Available from https://www.nhs.uk/conditions/endometriosis/
[12] NHS (2018) Fibroids [online]. NHS [viewed 08/10/2018]. Available from https://www.nhs.uk/conditions/fibroids/
[13] NHS (2016) Urinary Incontinence [online]. NHS [viewed 08/10/2018]. Available from https://www.nhs.uk/conditions/urinary-incontinence/
[14] Rawlings AV. Ethnic skin types: are there differences in skin structure and function? Int J Cosmet Sci. 2006;28(2):79–93.
[15] Setiawan, V.W., Pike, M.C., Kolonel, L.N., Nomura, A.M., Goodman, M.T., Henderson, B.E. (2007) Racial/Ethnic Differences in Endometrial Cancer Risk: The Multiethnic Cohort Study. American Journal of Epidemiology. 165(3), pp. 262-270.
[16] Taylor, S.C. (2002) Skin of color: biology, structure, function, and implications for dermatologie disease. J Am Acad Dermatol. 46(2 Suppl Understanding), S41–S62.
[17] Tinelli, A., Malvasi, A., Rahimi, S., Negro, R., Vergara, D., Martignago, R., Pellegrino, M., Cavallotti, C. (2010) Age-Related Pelvic Floor Modifications and Prolapse Risk Factors in Postmenopausal Women [Review]. Menopause: The Journal of The North American Menopause Society, 17(1), pp. 204-212.
[18] Thom, D.H., van den Eeden, S.K., Ragins, A.I., Wassel-Fyr, C., Vittinghof, E., Subak, L.L., Brown, J.S. (2006) Differences in Prevalence of Urinary Incontinence by Race/Ethnicity. Journal of Urology. 175(1), pp. 259-264.
[19] Vashi, N.A., Buainain De Castro Maymone, M., Kundu, R.V. (2016) Aging Differences in Ethnic Skin. Journal of Clinical and Aesthetic Dermatology. 9(1), pp. 31-38.
[20] Whitcomb, E.L., Rortveit, G., Brown, J.S., Creasman, J.M., Thom, D.H., Van Den Eeden, S.K., Subak, L.L. (2009) Racial Differences in Pelvic Organ Prolapse. Journal of Obstetrics and Gynecology. 114(6), pp. 1271-1277.