
Haemorrhoids are anal swellings that are more commonly known as piles. Around 50% of the UK population will likely develop one or more haemorrhoid at some stage. The symptoms associated with these can be painful, however read on to find out how Kegel8 can offer a simple solution.
What Causes Piles?
Haemorrhoids are abnormally enlarged vascular mucosal cushions in the anal canal. Mucosal cushions help us to maintain anal continence but when they become swollen, enlarged and start to cause symptoms, they then become haemorrhoids.
Sometimes piles can occur randomly, and they can happen to anyone; male or female, young or old. However, constipation is thought to be a trigger for piles as the straining can put pressure on the blood vessels in that area.
Straining during bowel movements is a huge risk factor for piles, so avoid it as much as you can (read on to learn how Kegel8 can help). Your age, pregnancy, and diet can affect your risk of developing piles.
What are the Symptoms of Piles?
- Bright-red, painless rectal bleeding when you pass stool
- Anal itching and irritation
- Soiling due to mucous discharge or incontinence
- A feeling of rectal fullness, discomfort or incomplete emptying of bowel movements
- Pain if a haemorrhoid prolapses and becomes strangulated
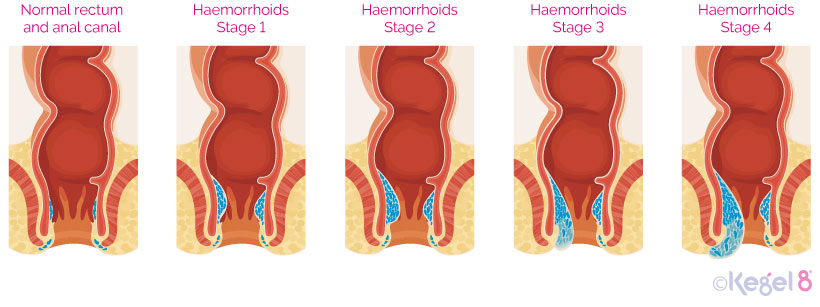
What are the Different Stages of Piles?
- Stage One – Small swellings on the inside of the anus. These aren’t visible from the outside and heal themselves with minor treatment.
- Stage Two – These are larger swellings that may appear when you go to the toilet but then disappear back inside again. These can also be cured with minor treatment.
- Stage Three – More severe small lumps that are visible from the outside of the anus and hang down, but they can be pushed back inside. May require treatment if painful.
- Stage Four – Most severe type of piles. Large lumps that hang down outside the anus. They cannot be pushed back inside and often require major treatment.
How Can You Prevent Piles?
- Kegel - Pelvic floor exercises can help prevent haemorrhoids by increasing blood flow to the anal region and improve circulation.
- Eat high-fibre foods - Eating food like fruit, veg and wholegrains can help soften your stool.
- Don't strain - If you strain whilst trying to pass stool you create a great deal of pressure on the veins in the anus.
- Go when you need to - If you hold off from passing your bowel movement and the urge disappears, your stool can become dry and harder to pass.
- Avoid long periods of sitting - Sitting for a long period of time, especially on the toilet, can increase pressure on the veins inside your anus.
Treating Stage One and Two Haemorrhoids:
- Kegel exercises – Pelvic floor exercises can improve circulation – bad blood circulation contributes to developing haemorrhoids.
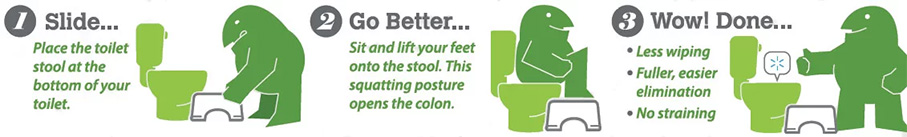
- Toilet stool – A stool allows your body to be in the prime position for total ease of bowel elimination.
- Hydrate – Drink plenty of water to keep your movements soft and regular.
- Fibre – Increase the amount of fibre in your diet by eating wholegrain breads, cereals, fruit and vegetables.
Treating Mild Haemorrhoids:
- Kegel – Kegels strengthen your pelvic floor muscles which helps provide good support for internal haemorrhoids and prevent existing ones from protruding.
- Moist toilet paper - To cleanse your anal region. Try to pat the area rather than rubbing.
- Sitz bath - A warm bath with Epsom salts can help soothe the irritation and reduce pain caused by haemorrhoids. Epsom salts can also be taken orally to naturally cure constipation and regulate bowel movements.
- Over-the-counter creams – Creams can help with symptoms such as inflammation and itching.
- Corticosteroid Creams – These can be prescribed by your GP if inflammation is bad but should only be used for a week.
- Painkillers – If your piles are painful you can take over-the-counter painkillers or see your GP for a prescription for painkilling cream.
- Laxatives – Constipation can make your piles worse. You can take over-the-counter laxatives or see your GP for a prescription.
Treating Severe Haemorrhoids:
Your doctor may refer you for a surgical procedure to help treat your haemorrhoids if they do not respond to regular treatment methods. Surgical treatments include:
- Banding – Used to treat third-degree piles. A tight elastic band is placed around the base of your haemorrhoid to cut off blood supply. Within 7 days, the haemorrhoid should drop off. This is usually performed with local anaesthetic and most people return to work the next day, although you may experience some pain or discomfort for a few days.
- Sclerotherapy – A chemical is injected directly into your blood vessels in the back passage. This works short-term by numbing nerve endings which should relieve pain, it also works to harden the haemorrhoid so that after 4-6 weeks it should shrink. Avoid exercise for a day or so afterwards. You may feel minor pain, but most people return to work the next day.
- Haemorrhoidectomy – For severe third and fourth-degree haemorrhoids, surgery is often recommended if other treatments are not successful. It is carried out under general anaesthetic and you will need a week or so off work to recover.
With a few simple lifestyle changes and Kegel8 exercises, you can help free yourself from pain, itching and embarrassment of haemorrhoids and piles.
Disclaimer: The information provided here is for your information only. It is not a substitute for professional medical advice, and it should not be used to diagnose or treat a health problem or disease. Please consult your GP if you have any questions or concerns.
Sources
[1] Fox A, Tietze PH, Ramakrishnan K. (2014) Anorectal conditions: hemorrhoids. FP Essentials, 419, pp. 11–19.
[2] King’s College Hospital (2016) Haemorrhoids (Piles): Information for Patients [online]. NHS Foundation Trust [viewed 04/10/2018].
[3] Mayo Clinic (2018) Hemorrhoids [online]. Mayo Clinic [viewed 05/10/2018]. Available from https://www.mayoclinic.org/diseases-conditions/hemorrhoids/symptoms-causes/syc-20360268
[4] Medline Plus (2018). Hemorrhoids [online]. Medline Plus [viewed 04/10/2018].
[5] NICE (2016) Haemorrhoids [online]. National Institute for Health and Care Excellence [viewed 04/10/2018]. Available from https://cks.nice.org.uk/haemorrhoids
[6] Tidy, Dr. C. (2017) Haemorrhoids: Piles [online]. Patient [viewed 04/10/2018]. Available from https://patient.info/doctor/haemorrhoids-piles-pro










